[:en]

After the skin is injured, in certain cases the healing process can leave a raised or a depressed scar. However, not all wounds will leave a scar. Normally very superficial wounds do not leave scars, provided that the healing process is smooth and there are not significant infections. It is important to understand that generally, scars develop when a certain degree of damage to the dermis has been caused either by an injury or infection. The scar is a normal reaction to the damage caused to the dermis.
In case of deep wounds (ie deep cuts, like those of serious accidents or surgical procedures) they usually develop into some form of scarring even if the healing process is smooth and free of infections. This is because in deep wounds the deeper part of the dermis (hypodermis) is usually affected and whenever the hypodermis is injured in some way the healing process will eventually lead to some degree of scarring, despite the way the wound has healed.
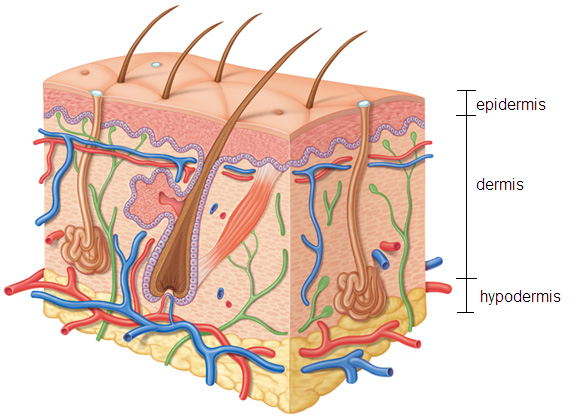
Figure 1. Whenever the dermis or the hypodermis are affected by an injury the wound will eventually develop into a certain degree of scarring.
In case the injury only involves the upper part of the dermis, if the wound heals speedily and appropriate after-care is followed then the likelihood of developing a scar decreases dramatically.
On the other hand, even a superficial wound can develop into a fully fledged hypertrophic scar if infections arise and persist over a long period of time. This is because the longer the infection persists the higher the likelihood of a certain degree of damage to be caused to the dermis. Sometimes a scar is hypertrophic (thickened/raised), or atrophic (depressed), but always confined to the margin of the original wound or injury. Hypertrophic scars, initially tend to be redder and often regress spontaneously (a process which can take one year or more).

Figure 2. Example of Hypertrophic Scar. Picture was taken soon after the healing was over. The scar is still pinker than the rest of the skin. The Scar is also confined to the borders of the original wound.
Hypertrophic scars develop during the wound healing process and not only do they stop growing when the healing process is over, but also they decrease in size over time by their own accord. Hypertrophic scar removal treatment, such as cortisone injections (steroids), can speed up this natural scar shrinkage process. Also, hypertrophic scar removal is relatively easy by using most ablative methods including lasers, electrical arcing, surgical excision and other methods. This is because the hypertrophic scars will not tend to grow back.

Figure 3. Another example of a recently formed hypertrophic scar. These types of scars are very easily removed by using most ablative methods in aesthetics, including lasers and electrical arcing. They do not tend to redevelop when removed.
Keloids, by contrast, may start sometime after a cutaneous injury of any type including normal acne, minor burns, chickenpox, ear piercing and piercings in general, minor scratches, surgical incision, injections, tattooing, laser aesthetic treatments including skin tightening, more in general any event which will trigger the skin regeneration process. They can also develop after some minor inflammation. Often Keloids can be mistaken for hypertrophic scars and vice versa. Keloids tend to extend beyond the wound site. This tendency to migrate into surrounding areas that weren't injured originally distinguishes Keloids from hypertrophic scars. Also, another difference between Keloids and hypertrophic scars is that Hypertrophic scars are formed during the healing process and stop developing as soon as the area has healed, on the other hand, Keloids do not stop growing when the healing process is over. Sometimes Keloids keep growing weeks after the original injury has healed.

Figure 4. One of the reasons Keloids appear often on the earlobes is due to ear piercing. This picture illustrates clearly how Keloidal formations tend to grow well beyond the original boundaries of the original injury which caused it.
Keloids "per se" are benign and non-dangerous growths, however, they can be compared to benign tumours due to their tendency to sustain growth after their initial formation. In case the growth seems disproportionate and persists over the period of several weeks leading to abnormal (irregular) shapes and disproportionate dimensions, like in case of formations displayed in Figure 4 for example, then excision for a histological examination is recommended. This is to make sure the growth although abnormal is benign. Please bear in mind that there is no scientifically proven connection between Keloidal formations and dangerous growths.

Figure 5. A classic example of unintended Keloidal formation after a tattooing treatment.

Figure 6. Keloidal formations after heart surgery. The suture points are demarcated by the clear keloids.
The difference between a classic Keloidal formation and a Hypertrophic scar is noted by comparing Figure 5 with Figure 2 and 3. The Keloidal formation in Figure 5 is clearly protruding and it does not present the normal pinkish colour of a normal Hypertrophic scar which is clearly confined within the borders of the original injury. Also in figure 5, it is possible to notice how the Keloidal formation is overgrowing in a similar fashion to the ones in Figure 4. In Figure 6 on the left, we can appreciate the clear Keloidal formation after heart surgery. The Keloids also formed on the suture points.
The Hypertrophic scars, in contrast, are very well confined within the original boundaries of the wound that initially formed it (See Figure 2 and 3). Keloids affect both sexes equally, although the incidence in the young female population has been reported to be higher than in young males, probably reflecting the greater frequency of earlobe piercing among women. The frequency of Keloidal occurrence is 15 times higher in highly pigmented people (skin types 4, 5 and 6), therefore African, Asian and Indian descendant people have increased likelihood of Keloid occurrences. It is also shown that the tendency to form Keloids is familial, therefore if one of your ancestors had this tendency then you will be more likely to form Keloids.
While hypertrophic scars are very easily removed by using various ablation methods, including lasers, electrical arcing, cryotherapy, excision, chemical peels etc, the removal of keloidal formations can be challenging.
This is because, despite the fact that they are removed using the several ablation methods currently available including surgical excision, Keloids tend to "grow back" or even expand or increase in size after their removal. Unfortunately, there is no known treatment which can scientifically guarantee Keloids will not recur after the removal.

Figure 8. Keloidal formation excised surgically. The surgical removal alone may be futile as the Keloid will tend to grow back due to the injury caused by the surgery itself. Therefore a post-surgical treatment to prevent the Keloid to recur will be necessary.
Despite the method used to remove any Keloidal formation, if a preventative measure to avoid the Keloidal recurrence is not used the lesion will "grow back" or worse, even regrow larger. Therefore any form of ablation alone is not sufficient to remove this type of lesion, or may even be detrimental due to the natural tendency of Keloids to develop and expand after a traumatic event to the skin. The methods used to prevent the regrowth of the Keloid after their removal using ablative methods are Cortisone or Fluorouracil superficial injections, Radio Therapy and others. These regrowths preventative methods are applied soon after the Keloid removal procedure using ablative any methods (ie lasers, electrical arcing, cryotherapy, surgical excision, chemical peels etc).
This is because any ablative method inevitably causes a skin traumatic event which will, in turn, trigger the Keloidal growth. For this reason, any effective treatment has to focus on having the Keloids to stop growing back after their removal.
No single regrowth preventative treatment is best for all Keloids because they may react differently to different treatments. The Keloid location, size, depth of the lesion, the age of the person, and the past response to the removal treatment may determine the best type of removal treatment.
One of the most known and economical methods to reduce the size of Keloidal formations is the use of injectable (steroids) cortisone, directly administered into the lesion. In most cases, this alone has been shown to reduce the size of the Keloidal formations without the use of any other ablative methods. As we know ablative methods of any type bear an inherent likelihood of Keloid recurrence as well as the potential increase in the size of the Keloid itself.
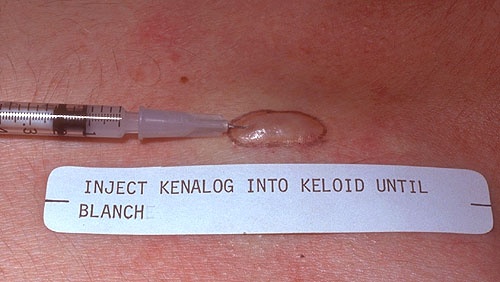
Figure 9. "Kenalog" is a brand name for "Triamcinolone Acetonide" which is a synthetic corticosteroid used to treat various skin conditions. In this image, we can see how the needle has to be inserted into the Keloid.
Cortisone injections are administered into the Keloid at 6 weeks interval and after each session normally the Keloid will reduce progressively in size by its own accord. The advantage of using this method is primarily the wide availability of safe and suitable steroids on the market. Furthermore, the first steroid course of injections alone will provide a clear indication if the Keloid responds well to this type of treatment. The avoidance of invasive (surgical) and non-invasive (lasers or voltaic arcing) ablative techniques is a clear benefit the skin does not require to undergo any traumatic events which could trigger a Keloidal regrowth or enlargement. This type of treatment will consist of a number of cortisone injections into the Keloids made at four to six weeks interval. This treatment on its own will suffice to reduce the Keloid in size after each course of a cortisone injection.
The use of cortisone injections should be the first attempt to treat Keloidal formations. It is important to emphasise that if the Keloid responds well to this treatment alone, in most cases it is not recommended to use ablative methods to fine tune the results. This is because as we know the use of any ablative treatment bears the inherent likelihood of triggering a form or recurrence. Although this treatment is not always effective it has a very high success rate and it has low risks associated with it. The results are apparent from the first course of injections as seen in the figure below.
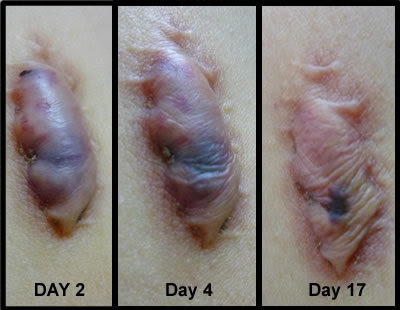
Figure 11. This picture clearly shows the efficacy of cortisone injections into the Keloid. Ablative treatments should be avoided if the Keloid responds well to this type of treatment.
Typical drugs used for this type of procedure:
- Triamcinolone acetonide
- Hydrocortisone
- Methylprednisolone
Typical Dosage:
5-10 mg/mL for developing Keloids and 10-40 mg/mL for a pre-existing, fully mature Keloid. The larger doses are usually used on bulky, mature Keloids.
The injections can be painful especially at high doses. Shots can be co-administered with a numbing agent (e.g., lidocaine) and/or after application of a topical numbing cream. Possible adverse side effects such as Hypopigmentation, Hyperpigmentation, dark red blotches, or tissue atrophy. Tissue atrophy looks like indentations in the skin and can occur with large amounts of steroids and/or injection in the surrounding normal tissue. Generally, Hypopigmentation may be reversible over time (it may take up to a year), however, tissue and fat atrophy can be permanent. Cushing’s syndrome can develop if too much steroid is used haphazardly.
Remember that the likelihood of side effects can be minimised but never completely avoided. Of course, if this treatment is effective, varying the dosage per session will determine the number of treatments required to achieve a satisfactory outcome. However, it is advisable to administer lower doses than normally possible and increase the number of sessions in order to minimise the likelihood of undesirable effects.
In case intra-lesion steroid injections are not effective, then the use of ablative treatments combined with recurrence prevention treatments can be the next step forward. As stated previously the use of ablative treatments (both invasive, like surgery, and non-invasive, like a laser and voltaic arcing treatments) should be avoided in the first instance due to the inherent likelihood of triggering recurrence or further growths.
However, the use of Lasers and voltaic arcing coupled with steroid treatments, radiation therapy or other treatments to prevent recurrence can be very effective. The regrowth preventative treatment is normally carried out after the Keloidal ablation has taken place.
In case the practitioner decides to use injectable steroids as a recurrence preventative measure, it is recommended to administer the steroid injections into the Keloid before the ablative treatment and then proceed to the physical removal of the Keloid by using, surgical excision, laser ablations or the electrical arcing. At the end of the Removal treatment then another course of superficial injections should be administered to both the treated and the surrounding area to further minimise the recurrence rate.
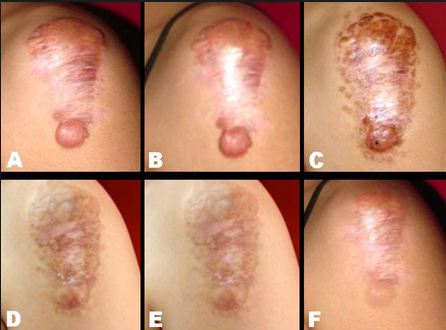
Figure 12. The stages of Keloid removal over time. Keloids are not always straightforward to remove,
In case of the use of radiation therapy to minimise the recurrence rate, this has to be used only at the end of the ablative treatment.
The use of combined treatments bears the inherent advantage of being able to remove the Keloid within one sitting, provided that the Keloid will not recur after the healing process. Once again combined treatments should be used only as the last resort or if the client prefers it (The client should be informed about all suitable available options for Keloid removal to make an informed decision).
Type of Ablative treatments suitable for Keloid removal, in case intra-lesional corticosteroid injections did not achieve the desired results, are :
- Lasers (by vaporising the Keloid) coupled with preventative measures to minimise recurrence.
- Voltaic Arcing (vaporisation) coupled with preventative measures to minimise recurrence.
- Surgical Excision coupled with preventative measures to minimise recurrence.
- Cryotherapy combined with preventative measures to minimise recurrence.
- Micro dermal abrasion combined with preventative measures to minimise recurrence.
Any ablative method on its own bear's high likelihood of triggering Keloid recurrence and therefore a form of Keloid recurrence preventative treatment should be used at least immediately after the Keloid removal.
Recurrence preventative measures:
- The most common Keloid recurrence minimisation method is the use of corticosteroid injections after any of these types of ablative treatments. This is due to the availability, efficacy and relatively low side effects of these drugs. In most cases, the injections are administered both before the ablation treatment directly into the Keloid and after the removal treatment into the surrounding area using superficial infiltrations.
- The use of Radiotherapy and other methods have been proved to be also effective.

Figure 13. Occlusion using Silicon sheets as a recurrence preventative measure after Keloid laser removal treatment.
- A particular study also suggests the use of Silicon Gel Sheeting up to 48 hours after an ablative treatment as a means of reducing the likelihood of recurrence. As the results are not always satisfactory this is not a first line preventative therapeutic treatment recommendable after Keloid ablative treatments. Click Here to learn more.
- Other promising Keloid recurrence preventative therapies after removal using ablative treatments include antiangiogenic factors, including vascular endothelial growth factor (VEGF) inhibitors (eg, bevacizumab), phototherapy (photodynamic therapy, UVA-1 therapy, narrowband UVB therapy), transforming growth factor (TGF)–beta3, tumor necrosis factor (TNF)-alpha inhibitors (etanercept), and recombinant human interleukin (rhIL-10), which are directed at decreasing collagen synthesis.
A useful table detailing the various type of treatments available for Keloid removal combined with regrowth prevention therapies, mentioning also the likelihood of recurrence can be found HERE.
Home treatments should not involve cutting, sanding, constricting the keloids with strings or rubber bands, or using any other method that traumatizes the skin. Doing so can increase the likelihood of recurrence, infections or keloid enlargement.
Use care when attempting home remedies for Keloid removal. Safe and effective remedies to shrink Keloids include occlusion (silicone pads or gel) and/or the application of certain substances. Please note that despite the fact that the proposed treatments are scientifically proven to improve the appearance of Keloids over time, several treatments, over a long time period are usually required in order to achieve the desired results. The duration of the treatment depends on the method used. The following home treatments are also effective in the treatment of normal Hypertrophic scars. Dramatic results are only currently achievable using intra-lesional corticosteroid injections or ablative methods combined with recurrence preventative treatments.
Silicone sheeting (Simple occlusion).
Occlusion in the treatment of scarring of any type has been used for several years. Occlusion can be performed in several ways, one of the ways which have been widely used is the application of Silicone adhesive sheets or appropriate silicon gel. Also, silicon gel sheets have been used to prevent new Keloids from forming following an injury or surgical operations. This is a treatment that can lead to eventual improvement in the appearance of both Hypertrophic scars and Keloids.
Figure 14. Occlusion applied on Keloid formations sustained over months for over 10 hours a day has been shown to be effective. however, this treatment is seldom viable for most people due to the impracticality of applying occlusion over long periods of time.
However, the use of sheeting has to be endured over several months (usually over six) in order for the results to become apparent. Therefore this type of treatment although ultimately effective is unsustainable for most people as this requires forming a new daily habit which needs to be sustained over months and this is rarely accomplished. Most "ad hoc" products are silicon gel sheets, or "scar sheets" which are self-adhesive, and reusable. They are applied to existing scars and Keloids to reduce their size and appearance over time. Silicon sheets should be worn over them for at least 10 hours per day for several months in order to achieve the desired results.
Figure 15. Several silicon products are available on the market. They must be worn for over 10 hours a day. The treatment has to be endured for over six months in order to achieve good results.
Silicon gel sheets are widely available on the market and can be bought at most pharmacies and many online retailers.
Vitamin E Coupled with Occlusion.

Figure 16. It has been shown how administering Vitamin E into the Keloid or Hypertrophic scar using the right topical solutions can lead to the eventual shrinkage of the lesion.
The use of topical Vitamin E based products (gel, oil, and ointments) have been shown a real efficacy in the eventual reduction in the size of the Keloid over a long period of time (several months). Therefore this solution on its own is not suitable for most people, because the use of this type of products can hardly be sustained over long periods. Likewise, as we know, the main problem with occlusion, used on its own, is the impracticality of wearing silicon sheets or gel products over long periods during the day (over 10 hours per day) and over sustained long periods of time (over 6 months). However, the combination of occlusion and the use of Vitamin E based products appears to be far more practical as the results are achieved much faster, usually within 2 months with an appropriate everyday use.
The reason for silicon occlusion to be effective in the treatment of Keloids is the "direct action on the fibroblasts and a hyperhydration of Subcutaneous tissue". Because generally the use of occlusion in aesthetic is successfully used for amplifying the subcutaneous delivery of active substances. Therefore applying Vitamin E on to the Keloid coupled with the occlusion effect of silicone sheets speeds up the Keloidal shrinkage process which would otherwise be possible. To view the related scientific study showing the efficacy of Vitamin E coupled with occlusion in Hypertrophic scar and Keloid treatment please Click Here. Please note that results vary according to the type of topical Vitamin E based product, time of occlusion carried out during the day.
Keloids are fundamentally different from Hypertrophic scars. Keloid removal treatment is not always simple as it is in the case of hypertrophic scars.This is because, unlike Hypertrophic scars, Keloids tend to "grow back" after any ablative treatment.
There are two main types of possible effective treatments:
- Professional. The first line of treatment is the use of Intralesional corticosteroid injections. Failing that the preferred option is the use of ablative treatments (Physical removal of the Keloids) combined with some other recurrence inhibition treatment. There are also several other options, however, they are not frequently used yet.
- Home treatments. The most successful type of home treatment is the use of suitable Vitamin E topical products, combined with occlusion. If carried out appropriately, this type of treatment has been shown to reduce the size of most Keloids within 2 months.
Both professional and home treatments are effective.
Professional treatments bear the advantage of allowing the Keloid removal with high success rate within one (or multiple) sitting(s) without the client needing to wear patches on his own. The main disadvantage is the higher costs and the potential side effects.
Home treatments are effective however, this does require the sustained daily use of Vitamin E based product coupled with occlusion over an extended period of time during the day and over several weeks. The main advantage is the lower costs and the very low likelihood of side effects.
[:es]

Después de que la piel se lesiona, en ciertos casos el proceso de curación puede dejar una cicatriz elevada o deprimida. Sin embargo, no todas las heridas dejarán cicatriz. Normalmente, las heridas muy superficiales no dejan cicatrices, siempre que el proceso de curación sea suave y no haya infecciones significativas. Es importante comprender que, en general, las cicatrices se desarrollan cuando un cierto grado de daño a la dermis se debe a una lesión o infección. La cicatriz es una reacción normal al daño causado a la dermis.
En el caso de heridas profundas (es decir, cortes profundos, como los de accidentes graves o procedimientos quirúrgicos), por lo general se convierten en alguna forma de cicatrización, incluso si el proceso de curación es suave y libre de infecciones. Esto se debe a que, en las heridas profundas, la parte más profunda de la dermis (hipodermis) generalmente se ve afectada y cada vez que la hipodermis se lesiona de alguna manera, el proceso de curación eventualmente conducirá a cierto grado de cicatrización, a pesar de la forma en que la herida ha cicatrizado.
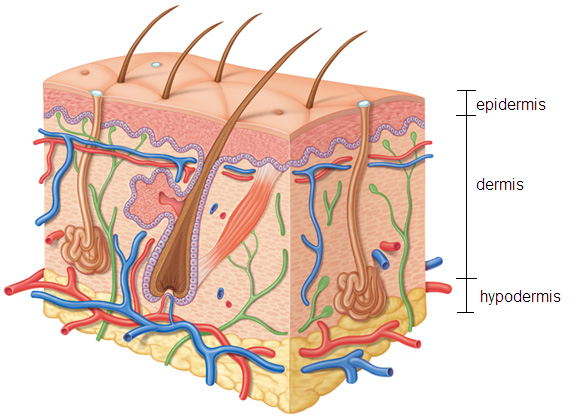
Figura 1. Cuando la dermis o la hipodermis se ven afectadas por una lesión, la herida eventualmente se convertirá en un cierto grado de cicatrización.
En caso de que la lesión solo afecte a la parte superior de la dermis, si la herida se cura rápidamente y se realiza un seguimiento posterior adecuado, la probabilidad de desarrollar una cicatriz disminuye drásticamente.
Por otro lado, incluso una herida superficial puede convertirse en una cicatriz hipertrófica de pleno derecho si las infecciones surgen y persisten durante un largo período de tiempo. Esto se debe a que cuanto más tiempo persiste la infección, mayor es la probabilidad de que se cause cierto daño a la dermis. A veces, una cicatriz es hipertrófica (engrosada / elevada) o atrófica (deprimida), pero siempre se limita al margen de la herida o lesión original. Las cicatrices hipertróficas, al principio tienden a ser más rojas ya menudo regresan espontáneamente (un proceso que puede durar un año o más).

Figura 2. Ejemplo de cicatriz hipertrófica. La foto fue tomada poco después de la curación. La cicatriz sigue siendo más rosada que el resto de la piel. La cicatriz también se limita a los bordes de la herida original.
Las cicatrices hipertróficas se desarrollan durante el proceso de cicatrización de la herida y no solo dejan de crecer cuando finaliza el proceso de curación, sino que también disminuyen de tamaño con el tiempo. El tratamiento de eliminación de cicatrices hipertróficas, como las inyecciones de cortisona (esteroides), puede acelerar este proceso natural de reducción de cicatrices. Además, la eliminación de cicatrices hipertróficas es relativamente fácil al usar la mayoría de los métodos ablativos, incluidos los láseres, los arcos eléctricos, la escisión quirúrgica y otros métodos. Esto se debe a que las cicatrices hipertróficas no tenderán a volver a crecer.

Figura 3. Otro ejemplo de una cicatriz hipertrófica recién formada. Estos tipos de cicatrices se eliminan muy fácilmente al usar la mayoría de los métodos ablativos en estética, incluidos los láseres y el arco eléctrico. No tienden a volver a desarrollarse cuando se eliminan.
Los queloides, por el contrario, pueden comenzar en algún momento después de una lesión cutánea de cualquier tipo, como acné normal, quemaduras leves, varicela, perforación de orejas y piercings en general, rasguños leves, incisión quirúrgica, inyecciones, tatuajes, tratamientos láser estéticos que incluyen estiramiento de la piel, más en General cualquier evento que desencadene el proceso de regeneración de la piel. También pueden desarrollarse después de alguna inflamación menor. A menudo, los queloides se pueden confundir con cicatrices hipertróficas y viceversa. Los queloides tienden a extenderse más allá del sitio de la herida. Esta tendencia a migrar a las áreas circundantes que no fueron lesionadas originalmente distingue a los queloides de las cicatrices hipertróficas. Además, otra diferencia entre los queloides y las cicatrices hipertróficas es que las cicatrices hipertróficas se forman durante el proceso de curación y dejan de desarrollarse tan pronto como el área se ha curado, por otro lado, los queloides no dejan de crecer cuando el proceso de curación ha terminado. A veces, los queloides continúan creciendo semanas después de que la lesión original haya cicatrizado.

Figura 4. Una de las razones por las que los queloides aparecen a menudo en los lóbulos de las orejas se debe a la perforación de la oreja. Esta imagen ilustra claramente cómo las formaciones queloidales tienden a crecer mucho más allá de los límites originales de la lesión original que la causó./caption]
Los queloides "per se" son crecimientos benignos y no peligrosos, sin embargo, pueden compararse con tumores benignos debido a su tendencia a sostener el crecimiento después de su formación inicial. En caso de que el crecimiento parezca desproporcionado y persista durante el período de varias semanas, lo que lleva a formas anormales (irregulares) y dimensiones desproporcionadas, como en el caso de las formaciones que se muestran en la Figura 4, por ejemplo, se recomienda la escisión para un examen histológico. Esto es para asegurarse de que el crecimiento, aunque anormal es benigno. Tenga en cuenta que no existe una conexión científicamente probada entre las formaciones queloideas y los crecimientos peligrosos.
[caption id="attachment_1183" align="aligncenter" width="431" class="center "] Figura 5. Un ejemplo clásico de formación queloidal no intencionada después de un tratamiento de tatuaje.
Figura 5. Un ejemplo clásico de formación queloidal no intencionada después de un tratamiento de tatuaje.
Figura 6. Formaciones queloides tras cirugía de corazón. Los puntos de sutura están demarcados por los queloides claros.
La diferencia entre una formación queloidal clásica y una cicatriz hipertrófica se observa al comparar la Figura 5 con la Figura 2 y la Figura 3. La formación queloidal en la Figura 5 es claramente sobresaliente y no presenta el color rosado normal de una cicatriz hipertrófica normal que está claramente limitada. Dentro de los límites de la lesión original. También en la figura 5, es posible observar cómo la formación queloidal está creciendo de manera similar a las de la figura 4. En la figura 6 de la izquierda, podemos apreciar la clara formación queloidal después de la cirugía cardíaca. Los queloides también se formaron en los puntos de sutura.
Las cicatrices hipertróficas, en contraste, están muy bien confinadas dentro de los límites originales de la herida que inicialmente la formaron (ver figuras 2 y 3). Los queloides afectan a ambos sexos por igual, aunque se ha informado que la incidencia en la población femenina joven es más alta que en los hombres jóvenes, lo que probablemente refleja la mayor frecuencia de perforación de la oreja entre las mujeres. La frecuencia de aparición de queloides es 15 veces mayor en las personas altamente pigmentadas (tipos de piel 4, 5 y 6), por lo que las personas afrodescendientes, asiáticas e indias tienen mayor probabilidad de aparición de queloides. También se muestra que la tendencia a formar queloides es familiar, por lo tanto, si uno de sus antepasados tuvo esta tendencia, es más probable que usted forme queloides.
Si bien las cicatrices hipertróficas se eliminan fácilmente mediante el uso de diversos métodos de ablación, incluidos los láseres, los arcos eléctricos, la crioterapia, la escisión, las exfoliaciones químicas, etc., la eliminación de las formaciones queloides puede ser un desafío

Figura 7. Queloides en el tipo de piel 1. Los queloides rara vez afectan los tipos de piel más claros.
Esto se debe a que, a pesar del hecho de que se eliminan utilizando los diversos métodos de ablación disponibles actualmente, incluida la escisión quirúrgica, los queloides tienden a "volver a crecer" o incluso a expandirse o aumentar de tamaño después de su extracción. Desafortunadamente, no hay un tratamiento conocido que pueda garantizar científicamente que los queloides no se repitan después de la eliminación..

Figura 8. Formación queloidal extirpada quirúrgicamente. La extirpación quirúrgica sola puede ser inútil, ya que el queloide tenderá a crecer nuevamente debido a la lesión causada por la cirugía en sí. Por lo tanto, será necesario un tratamiento postquirúrgico para evitar que el queloide se repita.
A pesar del método utilizado para eliminar cualquier formación queloidal, si no se usa una medida preventiva para evitar el queloide recuerrentel, la lesión "volverá a crecer" o, peor aún, aumentará. Por lo tanto, cualquier forma de ablación por sí sola no es suficiente para eliminar este tipo de lesión, o incluso puede ser perjudicial debido a la tendencia natural de los queloides a desarrollarse y expandirse después de un evento traumático en la piel. Los métodos utilizados para prevenir el recrecimiento del queloide después de su eliminación utilizando métodos ablativos son las inyecciones superficiales de cortisona o fluorouracilo, la radioterapia y otros. Estos métodos preventivos de recrecimiento se aplican poco después del procedimiento de remoción de queloides utilizando métodos ablativos (es decir, láser, arcos eléctricos, crioterapia, escisión quirúrgica, exfoliaciones químicas, etc.).
Esto se debe a que cualquier método ablativo causa inevitablemente un evento traumático en la piel que, a su vez, desencadena el crecimiento queloidal. Por esta razón, cualquier tratamiento eficaz debe centrarse en hacer que los queloides dejen de volver a crecer después de su eliminación.
Ningún tratamiento preventivo de rebrote único es el mejor para todos los queloides porque pueden reaccionar de manera diferente a diferentes tratamientos. La ubicación del queloide, el tamaño, la profundidad de la lesión, la edad de la persona y la respuesta anterior al tratamiento de eliminación pueden determinar el mejor tipo de tratamiento de eliminación.
Uno de los métodos más conocidos y económicos para reducir el tamaño de las formaciones queloides es el uso de cortisona inyectable (esteroides), administrada directamente en la lesión. En la mayoría de los casos, solo se ha demostrado que reduce el tamaño de las formaciones queloides sin el uso de ningún otro método ablativo. Como sabemos, los métodos ablativos de cualquier tipo tienen una probabilidad inherente de recurrencia de queloides, así como el aumento potencial en el tamaño del propio queloide.
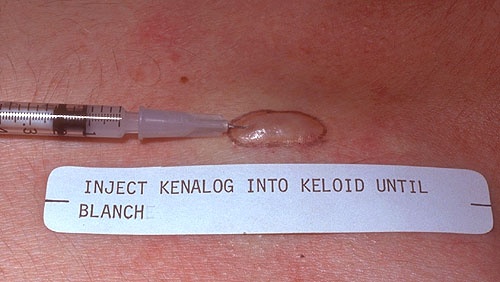
Figura 9. "Kenalog" es un nombre comercial de "Triamcinolone Acetonide", que es un corticosteroide sintético utilizado para tratar diversas afecciones de la piel. En esta imagen, podemos ver cómo se debe insertar la aguja en el queloide.
Las inyecciones de cortisona se administran en el queloide a intervalos de 6 semanas y, después de cada sesión, normalmente el queloide se reducirá progresivamente de tamaño por sí mismo. La ventaja de usar este método es principalmente la amplia disponibilidad de esteroides seguros y adecuados en el mercado. Además, el primer ciclo de inyecciones de esteroides solo proporcionará una indicación clara de si el queloide responde bien a este tipo de tratamiento. Evitar las técnicas de ablación invasivas (quirúrgicas) y no invasivas (láseres o arcos voltaicos) es un claro beneficio que la piel no requiere para experimentar eventos traumáticos que podrían desencadenar un recrecimiento o agrandamiento queloidal. Este tipo de tratamiento consistirá en una serie de inyecciones de cortisona en los queloides a intervalos de cuatro a seis semanas. Este tratamiento por sí solo será suficiente para reducir el tamaño del queloide después de cada ciclo de inyección de cortisona.
El uso de inyecciones de cortisona debe ser el primer intento de tratar las formaciones queloideas. Es importante enfatizar que si el queloide responde bien a este tratamiento solo, en la mayoría de los casos no se recomienda usar métodos ablativos para ajustar los resultados. Esto se debe a que, como sabemos, el uso de cualquier tratamiento ablativo tiene la posibilidad inherente de desencadenar una forma o recurrencia. Aunque este tratamiento no siempre es eficaz, tiene una tasa de éxito muy alta y tiene bajos riesgos asociados. Los resultados son evidentes a partir del primer ciclo de inyecciones, como se ve en la siguiente figura.
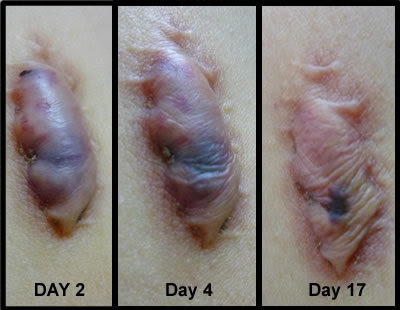
Figura 11. Esta imagen muestra claramente la eficacia de las inyecciones de cortisona en el queloide. Los tratamientos ablativos deben evitarse si el queloide responde bien a este tipo de tratamiento.
Medicamentos típicos utilizados para este tipo de procedimiento:
- Acetónido de triamcinolona
- Hidrocortisona
- Metilprednisolona
Dosis típica:
5-10 mg / ml para desarrollar queloides y 10-40 mg / ml para un queloide completamente maduro preexistente. Las dosis más grandes se usan generalmente en queloides maduros y voluminosos.
Las inyecciones pueden ser dolorosas, especialmente a altas dosis. Las inyecciones pueden coadministrarse con un agente para adormecer (por ejemplo, lidocaína) y / o después de la aplicación de una crema para adormecer tópica. Posibles efectos secundarios adversos, como hipopigmentación, hiperpigmentación, manchas de color rojo oscuro o atrofia del tejido. La atrofia tisular se ve como hendiduras en la piel y puede ocurrir con grandes cantidades de esteroides y / o inyección en el tejido normal circundante. En general, la hipopigmentación puede ser reversible con el tiempo (puede tardar hasta un año), sin embargo, la atrofia del tejido y la grasa puede ser permanente. El síndrome de Cushing puede desarrollarse si se usa demasiado esteroide al azar.
Recuerde que la probabilidad de efectos secundarios se puede minimizar, pero nunca evitar por completo. Por supuesto, si este tratamiento es efectivo, la variación de la dosis por sesión determinará la cantidad de tratamientos necesarios para lograr un resultado satisfactorio. Sin embargo, es aconsejable administrar dosis más bajas de lo que normalmente es posible y aumentar el número de sesiones para minimizar la posibilidad de efectos no deseados.
En el caso de que las inyecciones de esteroides intra lesiones no sean efectivas, el siguiente paso es el uso de tratamientos ablativos combinados con tratamientos de prevención de recurrencias. Como se indicó anteriormente, el uso de tratamientos ablativos (tanto invasivos, como la cirugía, y no invasivos, como un láser y los tratamientos de arco voltaico) se debe evitar en primera instancia debido a la probabilidad inherente de desencadenar la recurrencia o nuevos crecimientos.
Sin embargo, el uso de láseres y arcos voltaicos junto con tratamientos con esteroides, radioterapia u otros tratamientos para prevenir la recurrencia puede ser muy efectivo. El tratamiento preventivo de rebrote se lleva a cabo normalmente después de la ablación queloidal.
En caso de que el profesional decida usar esteroides inyectables como medida preventiva de recurrencia, se recomienda administrar las inyecciones de esteroides en el queloide antes del tratamiento ablativo y luego proceder a la remoción física del queloide mediante escisión quirúrgica, ablación con láser o arcos electricos Al final del tratamiento de eliminación, debe administrarse otro ciclo de inyecciones superficiales tanto en el área tratada como en el área circundante para minimizar aún más la tasa de recurrencia.
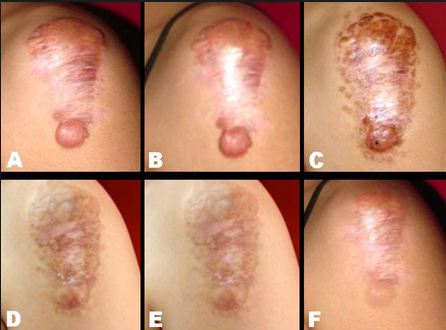
Figura 12. Las etapas de eliminación de queloides con el tiempo. Los queloides no siempre son fáciles de eliminar,
En el caso de que se use radioterapia para minimizar la tasa de recurrencia, debe usarse solo al final del tratamiento ablativo.
El uso de tratamientos combinados conlleva la ventaja inherente de poder eliminar el queloide en una sola sesión, siempre que el queloide no se repita después del proceso de curación. Una vez más, los tratamientos combinados deben usarse solo como último recurso o si el cliente lo prefiere (se debe informar al cliente sobre todas las opciones disponibles adecuadas para la eliminación de queloides para tomar una decisión informada).
Los tipos de tratamientos ablativos adecuados para la eliminación de queloides, en el caso de que las inyecciones de corticosteroides intra-lesionales no logren los resultados deseados, son:
- Láseres (al vaporizar el queloide) junto con medidas preventivas para minimizar la recurrencia.
- Arcop Voltaico (vaporización) junto con medidas preventivas para minimizar la recurrencia.
- Escisión quirúrgica combinada con medidas preventivas para minimizar la recurrencia.
- Crioterapia combinada con medidas preventivas para minimizar la recurrencia.
- La abrasión microdérmica combinada con medidas preventivas para minimizar la recurrencia.
Cualquier método ablativo sobre la alta probabilidad de desencadenar la recurrencia de queloides y, por lo tanto, una forma de tratamiento preventivo de recurrencia de queloides debe utilizarse al menos inmediatamente después de la eliminación de queloides.
Medidas preventivas de recurrencia:
- El método más común de minimización de la recurrencia del queloide es el uso de inyecciones de corticosteroides después de cualquiera de estos tipos de tratamientos ablativos. Esto se debe a la disponibilidad, eficacia y efectos secundarios relativamente bajos de estos medicamentos. En la mayoría de los casos, las inyecciones se administran tanto antes del tratamiento de ablación directamente en el queloide como después del tratamiento de extracción en el área circundante mediante infiltraciones superficiales.
- El uso de la radioterapia y otros métodos han demostrado ser también eficaces.

Figura 13. Oclusión con láminas de silicona como medida preventiva de recurrencia después del tratamiento de remoción con láser al queloide.
- Un estudio en particular también sugiere el uso de láminas de gel de silicona hasta 48 horas después de un tratamiento ablativo como medio para reducir la probabilidad de recurrencia. Como los resultados no siempre son satisfactorios, no es un tratamiento terapéutico preventivo de primera línea recomendable después de los tratamientos ablativos con queloides. Clic aquí para saber más.
- Otras terapias preventivas de recurrencia de queloides prometedoras después de la eliminación con tratamientos ablativos incluyen factores antiangiogénicos, incluidos los inhibidores del factor de crecimiento endotelial vascular (VEGF) (p. Ej., Bevacizumab), fototerapia (terapia fotodinámica, terapia UVA-1, terapia UVB de banda estrecha), factor de crecimiento transformante (TGF) ) - beta3, factor de necrosis tumoral (TNF) - inhibidores de alfa (etanercept) e interleucina humana recombinante (rhIL-10), que están dirigidos a disminuir la síntesis de colágeno.
se puede encontrar una tabla útil que detalla los diversos tipos de tratamientos disponibles para la eliminación de queloides combinados con terapias de prevención de recrecimiento, mencionando también la probabilidad de recurrencia.AQUÍ.
Los tratamientos en el hogar no deben incluir el corte, lijado, constricción de los queloides con cuerdas o bandas de goma, o el uso de cualquier otro método que traumatiza la piel. Hacerlo puede aumentar la probabilidad de recurrencia, infecciones o agrandamiento de los queloides..
Tenga cuidado al intentar remedios caseros para la eliminación de queloides. Los remedios seguros y efectivos para reducir los queloides incluyen la oclusión (almohadillas de silicona o gel) y / o la aplicación de ciertas sustancias. Tenga en cuenta que a pesar del hecho de que los tratamientos propuestos están científicamente probados para mejorar la apariencia de los queloides con el tiempo, generalmente se requieren varios tratamientos durante un largo período de tiempo para lograr los resultados deseados. La duración del tratamiento depende del método utilizado. Los siguientes tratamientos caseros también son efectivos en el tratamiento de cicatrices hipertróficas normales .En la actualidad, solo se pueden lograr resultados dramáticos con inyecciones de corticosteroides intra-lesionales o métodos ablativos combinados con tratamientos preventivos de recurrencia.
Láminas de silicona (oclusión simple).
La oclusión en el tratamiento de cicatrización de cualquier tipo se ha utilizado durante varios años. La oclusión se puede realizar de varias maneras, una de las formas que se ha utilizado ampliamente es la aplicación de láminas adhesivas de silicona o gel de silicona apropiado. Además, se han utilizado láminas de gel de silicona para evitar que se formen nuevos queloides después de una lesión u operaciones quirúrgicas. Este es un tratamiento que puede llevar a una mejora eventual en la aparición de cicatrices hipertróficas y queloides.
Figura 14. La oclusión aplicada en formaciones queloides sostenidas durante meses durante más de 10 horas al día ha demostrado ser eficaz. sin embargo, este tratamiento rara vez es viable para la mayoría de las personas debido a la imposibilidad de aplicar la oclusión durante largos períodos de tiempo.
Sin embargo, el uso de láminas debe ser soportado durante varios meses (generalmente más de seis) para que los resultados sean evidentes. Por lo tanto, este tipo de tratamiento, aunque en última instancia es efectivo, es insostenible para la mayoría de las personas, ya que esto requiere formar un nuevo hábito diario que debe mantenerse durante meses y esto rara vez se logra. La mayoría de los productos "ad hoc" son láminas de gel de silicona o "láminas cicatriciales" que son autoadhesivas y reutilizables. Se aplican a las cicatrices y queloides existentes para reducir su tamaño y apariencia a lo largo del tiempo. Las láminas de silicona se deben usar sobre ellas durante al menos 10 horas por día durante varios meses para lograr los resultados deseados.
Figura 15. Varios productos de silicona están disponibles en el mercado. Deben ser usados por más de 10 horas al día. El tratamiento debe durar más de seis meses para lograr buenos resultados.
Las láminas de gel de silicona están ampliamente disponibles en el mercado y se pueden comprar en la mayoría de las farmacias y en muchas tiendas minoristas en línea.
Vitamina E Acoplada Con Oclusión.

Figura 16. Se ha demostrado cómo la administración de vitamina E en la cicatriz queloide o hipertrófica con las soluciones tópicas correctas puede llevar a la eventual reducción de la lesión.
El uso de productos tópicos a base de vitamina E (gel, aceite y ungüentos) ha demostrado una eficacia real en la eventual reducción del tamaño del queloide durante un largo período de tiempo (varios meses). Por lo tanto, esta solución por sí sola no es adecuada para la mayoría de las personas, ya que el uso de este tipo de productos difícilmente puede mantenerse durante largos períodos. Del mismo modo, como sabemos, el principal problema de la oclusión, que se usa solo, es la impracticabilidad de usar láminas de silicona o productos de gel durante largos períodos durante el día (más de 10 horas por día) y durante largos períodos sostenidos (más de 6 meses). Sin embargo, la combinación de oclusión y el uso de productos a base de vitamina E parece ser mucho más práctica, ya que los resultados se logran mucho más rápido, generalmente dentro de 2 meses con un uso diario adecuado.
La razón para que la oclusión del silicio sea eficaz en el tratamiento de los queloides es la ""acción directa sobre los fibroblastos y la hiperhidratación del tejido subcutáneo"". Porque, en general, el uso de la oclusión en estética se usa con éxito para amplificar la administración subcutánea de sustancias activas. Por lo tanto, la aplicación de vitamina E en el queloide junto con el efecto de oclusión de las láminas de silicona acelera el proceso de contracción queloidal que de otra manera sería posible. Para ver el estudio científico relacionado que muestra la eficacia de la vitamina E junto con la oclusión en la cicatriz hipertrófica y el tratamiento con queloides, haga click aquí. Tenga en cuenta que los resultados varían según el tipo de producto tópico basado en vitamina E, el tiempo de oclusión realizado durante el día.
Los queloides son fundamentalmente diferentes de las cicatrices hipertróficas. El tratamiento de eliminación de queloides no siempre es simple como lo es en el caso de las cicatrices hipertróficas. Esto se debe a que, a diferencia de las cicatrices hipertróficas, los queloides tienden a "volver a crecer" después de cualquier tratamiento ablativo.
Hay dos tipos principales de posibles tratamientos efectivos:
- Profesional. La primera línea de tratamiento es el uso de inyecciones de corticosteroides intralesionales. En su defecto, la opción preferida es el uso de tratamientos ablativos (eliminación física de los queloides) combinados con algún otro tratamiento de inhibición de recurrencia. También hay varias otras opciones, sin embargo, todavía no se utilizan con frecuencia.
- Tratamientos a domicilio. El tipo más exitoso de tratamiento en el hogar es el uso de productos tópicos de vitamina E adecuados, combinados con oclusión. Si se lleva a cabo adecuadamente, se ha demostrado que este tipo de tratamiento reduce el tamaño de la mayoría de los queloides en 2 meses.
Tanto los tratamientos profesionales como los domiciliarios son efectivos.
Los tratamientos profesionales tienen la ventaja de permitir la eliminación de queloides con una alta tasa de éxito en una (o varias) sesiones sin que el cliente tenga que usar parches por su cuenta. La principal desventaja es el mayor costo y los posibles efectos secundarios.
Los tratamientos caseros son efectivos, sin embargo, esto requiere el uso diario sostenido de un producto a base de vitamina E junto con la oclusión durante un período prolongado de tiempo durante el día y durante varias semanas. La principal ventaja es el menor costo y la muy baja probabilidad de efectos secundarios.
[:]

